The science behind weight loss surgery never stops moving. Discussions between lap band and gastric sleeve (also called sleeve gastrectomy) have evolved considerably in recent years.
It is important to understand both procedures (gastric bypass and gastric sleeve) if you are thinking of starting your weight loss journey.
Today, we’ll talk about lap bands and sleeve gastrectomies, and why gastric sleeves are the most frequent recommended weight loss procedure here at Dr. Feiz & Associates.
Table of Contents |
The History of Bariatric Surgery
In the last 20 years, obesity has been an epidemic not only in the US, but all over the world. Finding an effective treatment has been a challenge for medical practitioners until the discovery of bariatric surgery in recent years. This has led to an increased success and novel insights on the pathophysiology of obesity.
If we were to go all the way back, there are historical reports that the very first bariatric surgery was performed around the 10th century in Spain. The patient was the late King of Leon, D. Sancho.
He was so obese that he couldn’t walk, ride a horse, or even pick up a sword. He couldn’t conduct simple activities that were expected from a king and this ultimately led to his dethronement.
He was then brought to a Jewish doctor, Hisdai ibn Shaprut, who sutured his mouth shut so he could only consume liquids with the help of straw. These liquids consisted of teriaca, opium and a variety of herbs. Sounds extreme, right?
This measure resulted in losing half of his initial weight and regaining his throne.
Well, for the past 50 years, surgeons have been working tirelessly to come up with different surgical techniques to aid the ever growing demand of the population for safer and more effective weight loss procedures.
Thanks to these surgeons, we do not have to sew our mouth shut to lose weight. What a time to be alive!
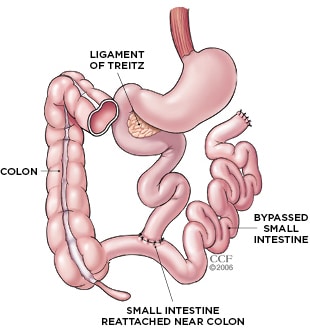
Jejunoileal Bypass: The Surgery of the Past
In the late 1960s, a new trend for weight loss emerged. At the time, Jejunoileal Bypass was the most effective approach for achieving and maintaining weight loss.
This approach, first introduced in 1954, created a surgically-induced short bowel syndrome. Though effective, this weight loss procedure is not safe at all.
This surgery is done to essentially bypass more than 90% of the functioning small intestine,and was presumed that this surgery would cause malabsorption that would then ultimately lead to weight loss.
Published by World Journal of Gastroenterology, a case report regarding jejunoileal bypass concluded that though the procedure was deemed effective and reliable in terms of weight loss, it was also associated with severe complications such as renal failure, diarrhea and consequent electrolyte imbalances, liver disease, fat-soluble vitamin deficiencies, malnutrition and death.
It’s just not worth it.
The Evolution of Bariatric Surgery: Gastric Bypass
After such devastating complications from jejunoileal bypass, medical practitioners have never been more eager to find the safest type of weight loss surgery.
Dr. Edward Mason, a surgeon from University of Iowa, noted that the patients who underwent gastrectomy for stomach cancer had shown a noticeable amount of weight loss.
From this thought, a safer and less invasive procedure was born - the gastric bypass.
Thanks to the ever evolving medical technology, a full on operation is now done with just 4 to 6 small cuts in the belly with the help of a camera. This procedure is called Roux-en-Y Gastric Bypass.
Emergence of Lap Band Surgery
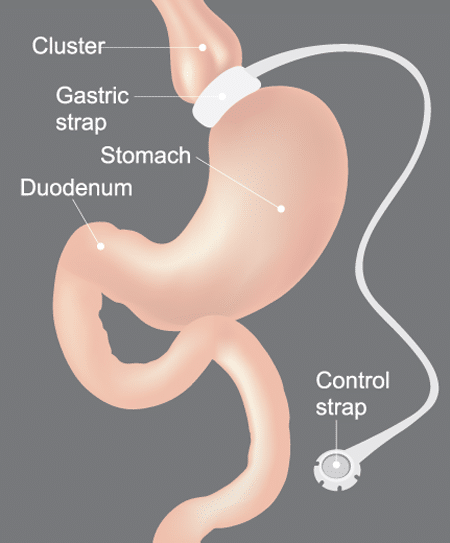
Lap Band or Gastric Band surgery is a procedure where your surgeon places an adjustable ring around the upper part of the stomach.
The band literally ties off most of the stomach, leaving only a very small available area. The result is that overeating becomes so uncomfortable that patients have every reason to avoid it, giving them plenty of negative reinforcement to avoid excessive eating.
As the gastric bypass became established, this much less invasive alternative was extremely attractive to many patients because it left the stomach entirely intact and could be reversed if necessary.
Banding has produced good results for many patients. However, major drawbacks were a lower success rate and a higher rate of complications.
Research published by JAMA Surgery found that 1 out of 5 Medicare beneficiaries who have undergone lap band surgery needed to have another operation during the average period of 4½ years.
These reoperations are usually needed due to complications and device malfunctions like band displacement and bowel obstruction.
Lap Band Pros & Cons
Minimally invasive and reversible.
Allows for some adjustment
Less consistently effective than other procedures.
Additional adjustments procedures are required.
The rate of complications may be higher.
Many patients end up seeking revisions to sleeve gastrectomies
All About Gastric Sleeve Surgery
Gastric Sleeve Surgery, or Vertical Sleeve Gastrectomy, permanently reduces the size of the stomach by roughly 75-85%.
It is much less radical than a bypass, primarily because it doesn’t change the actual workings of the digestive tract beyond reducing the stomach.
Over time, it has turned out that this type of procedure has been significantly more reliable than banding, largely because of the positive benefits of the operation.
Along with reducing the size of the stomach, the surgery also removes something called the fundus, which produces a hunger-associated hormone called ghrelin. This is important because obese people produce more ghrelin than others and the production of the hormone tends to increase as they lose weight.
When the body goes into a kind of starvation mode, more of these hormones are produced which sabotage the efforts to defeat obesity.
It has become very clear over the years that the two-fold impact of the sleeve procedure – making overeating unpleasant, while also reducing the drives that make us want to overeat in the first place – is a very powerful combination.
Pros & Cons Of Gastric Sleeve
Two-pronged impact – discourages overeating while lowering the appetite.
Less radical than the gastric bypass – alters only the size of the stomach.
As with other procedures, patients need to be careful to avoid overeating. The sleeve is much less radical than the gastric bypass but a complication called “dumping syndrome” – which is as unpleasant as it sounds – is still a risk.
A sleeve gastrectomy is irreversible.
“Should I get a lap band or should I get gastric sleeve surgery?”
Though these two procedures share the same goal of having the stomach hold less food, the approach for each is very different.
While we’ve already covered how these two procedures are done, below is a quick summary:
A lap band is a device that ties off most of the stomach, leaving only a very small available area for food.
A gastric sleeve involves actual removal of the large portion of the stomach.
Because sleeve gastrectomy involves cutting parts of the stomach, the recovery time for this procedure is generally longer than that of a lap band surgery.
Yes, gastric sleeve is more invasive. However, it provides superior weight loss in the first 12 to 18 months post-surgery.
Lap Band:
Severely obese adults who have been obese for at least five years and for whom non-surgical weight loss methods have not been successful.
Patients must have a Body Mass Index (BMI) of at least 40.
A BMI of at least 35 with one or more severe morbid (unhealthy) conditions
Or must be at least 100 pounds over their estimated ideal weight.
Gastric Sleeve:
Usually reserved for patients whose BMI is over 40.
Some studies have concluded that it is also safe for patients with lower BMI.
Lap Band:
(Source: PMC and JAMA Network)
20% of patients have needed to get a reoperation to get the band fixed or replaced or have even had to get another weight loss procedure.
The average number of procedures per lap band patient.
Only 11.2% have achieved satisfactory weight loss.
86% of patients were still suffering from obesity after the procedure.
22% of patients in a study regained their weight or even exceeded it.
54% of patients had it removed due to complications.
Gastric Sleeve:
(Source: JAMA Network)
76.8% of patients show excessive weight loss in the 12-18 months after surgery.
64.5% of diabetic patients did not need to take medications 1 year post-surgery.
50.7% of the people who stopped taking their diabetes medications were able to stay in complete remission.
There's a 77.8% remission rate for people who had hypertension before the operation.
“So, which is better? Lap band or gastric sleeve?”
With these numbers provided, it is safe to conclude that sleeve gastrectomy is the best option amongst the two. Though more invasive and has a longer recovery time, gastric sleeve is way more effective with less probability of reoperation and complication.
Several studies cited in this article confirmed that sleeve gastrectomy is more effective in weight loss than adjustable gastric banding in the long run. When making a decision which procedure to get, don’t keep your focus on just losing weight, but also on the weight maintenance for the years to come.
¿Sientes que lo has intentado todo para adelgazar? ¿Ya se sometió a una cirugía de pérdida de peso sin éxito? El Dr. Michael Feiz y su equipo le proporcionarán toda la información y los recursos que necesita para tomar una decisión informada sobre la cirugía para bajar de peso. Aunque los detalles varían de un paciente a otro, estaremos con usted en cada paso del camino. De la cirugía—> a la recuperación—> ¡a un estilo de vida saludable permanente!
Vea el video a continuación de una historia única de una familia que se sometió a una cirugía para bajar de peso. Vea el antes y el después de la cirugía de pérdida de peso y cómo lo experimentaron. Estas historias no son inusuales y nos complace decir que la mayoría de nuestros pacientes descubren que pueden mantener su pérdida de peso con la ayuda de un procedimiento seleccionado especialmente para ellos.